Researching Symptoms of an Undiagnosed Disease
When my daughter, Rylae-Ann, was about 3 months old, she wasn’t meeting her milestones. Then came the “spells,” which we thought were seizures. These unknown occurrences were followed by misdiagnoses and several hospital admissions.
My wife, Judy, and I were uncertain about the initial diagnoses. We weren’t getting answers, so we ignored the warnings against Googling symptoms and began searching the internet. One result led me to an article about a Canadian girl who had a rare disorder with similar symptoms, but I dismissed it because it was ultra-rare. It took another article shared on Facebook for my wife and me to inform the doctors that we believed our daughter had aromatic l-amino acid decarboxylase (AADC) deficiency.
A genetic test confirmed it, but searching online helped us receive a prompter diagnosis. Recently I retraced my digital footprints by entering the search terms I used when trying to find out what my daughter had. They were layman’s terms that simply described what I saw. This time, those same search terms did not result in any information about AADC deficiency on the first page of Google.
This column aims to reach concerned parents who are vigorously searching for answers online. By crowdsourcing search terms of common AADC symptoms from our community, I have compiled a list that will hopefully land this column among the top results for anyone searching for answers.
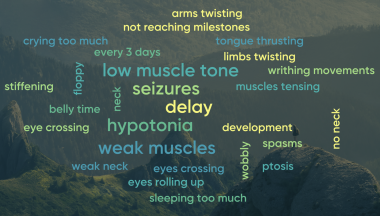
A word cloud Richard created using crowdsourced terms from the AADC deficiency community. (Courtesy of Richard E. Poulin III)
Not reaching milestones and developmental delays
When Rylae was born, we had our baby guidebooks already read and pages dog-eared. We were eager to get her moving through the milestones listed and even excel beyond them. However, she didn’t do much in her first few months.
We needed to cradle her with extra support, but this did not raise any red flags. Looking back on those first few months, we were bothered that she couldn’t do belly time. When we placed her on her belly, she would scream face down. Her cries of distress were muffled by the mattress. We worried about her not breathing, so we kept her on her back. I felt like I always had one eye open when she slept because I feared that if she accidentally rolled over, she wouldn’t be able to roll back.
Another milestone that concerned us was that she was not reaching out and grabbing. We had a plethora of shiny colorful toys that screamed for a baby’s attention. However, Rylae never seemed interested. The milestone of grabbing her feet also passed, but we never looked beyond that one. She was at a standstill in her progress.

Despite showing Rylae-Ann toys, she would not reach out and grab them or our hands. (Photo by Richard E. Poulin III)
Hypotonia, or a floppy baby with weak muscles
Our baby was born perfect, without complications. In hindsight, we noticed our newborn was floppy. We didn’t think much of it, but we warned our family to be extra careful before handing her over. She was floppy compared to our friend’s newborn baby and didn’t yet have the strength that other newborns did. We continued to help her reach her milestones.
When she was about 3 months old, we started to make a concentrated effort to help her strengthen her muscles. She couldn’t keep her head upright. Her limbs felt like Jell-O compared to the sinewy fibers that were more noticeable when holding other babies.
The symptom we call floppy baby is known as hypotonia. A child with hypotonia is characterized as having low muscle tone. Despite being floppy, her joints did not move freely.

We were very concerned when we first saw Rylae-Ann crossing her eyes and thrusting her tongue. (Photo by Richard E. Poulin III)
Seizurelike spells every three days
We knew something wasn’t right when we began to see events similar to seizures. We called them spells, and strangely they happened like clockwork. Every three days in the evening, an attack would happen. At first, they were short, and I thought they might be muscle spasms from pushing our daughter to achieve her developmental milestones.
Over time, they began to last longer. The spells still happened every three days, but the intensity also became more concerning. We were able to minimize the severity or have her snap out of it briefly. This, combined with the cyclical nature, left us thinking the attacks weren’t seizures.
After Rylae was diagnosed, we learned that these events are a characteristic symptom of AADC deficiency. Our theories were confirmed that they were not seizures but instead an eye movement disorder known as oculogyric crises (OGCs). Rylae-Ann’s eyes would involuntarily stay crossed or go upward.
OGCs are a side effect of the neurotransmitter disorder, since sufferers are unable to synthesize dopamine and serotonin.
Her eyes would remain in this state during the spell, unable to move. Her mouth would pucker, and her tongue would do a thrusting action. Her tongue would continue going in and out of her mouth while she breathed heavily. An OGC was the only time it felt like she had muscles.
Anxiety and emotional outbursts often announced the end of the attack. It was the only time we were happy to hear her cry.

During an attack, an EEG showed her brainwaves were normal, but Rylae-Ann’s eyes, tongue, arms, and leg would tense and twist in uncontrollable movements. (Photo by Richard E. Poulin III)
The neck
We had to support Rylae’s neck with pillows similar to what you would use on an airplane. I worried she had a short neck in the first few months of life. My first round of searching the internet worried me that she had torticollis, a medical issue described as having weak neck muscles.
We worked to try to strengthen her neck muscles, but without assistance from us or pillows, she couldn’t keep her head upright.

We place pillows around Rylae-Ann to support her neck and body while placing toys in her hands to help her feel the sensation. (Photo by Richard E. Poulin III)
Twisting legs and tense muscles
During an OGC, her arms and legs would stiffen, and her limbs would twist inward. Her hands would form tight fists while her toes were angled down. She would make this writhing movement for long periods lasting several hours.
When we described this to the doctor, they diagnosed her with dystonia, a movement disorder that causes muscles to contract involuntarily and move in repetitive twisting motions. We believe that this movement disorder, combined with her weak, immobile state, led to her having a dislocated hip.

Rylae-Ann cried excessively and would often wake from her sleep crying. (Photo by Richard E. Poulin III)
Crying and anxiety
Newborns cry. However, it seemed like Rylae was crying constantly for the first year. I thought I was going crazy from the lack of sleep. Judy and I tried to work in shifts, waking to soothe and care for Rylae when she woke, but there was no sleeping through the loud cries.
Whenever Rylae was exposed to a new environment or a new face, she would instantly cry as well. This seemed related to anxiety, and later, we confirmed this was true. We no longer desired to parade Rylae around town. A kind person coming up to comment on how cute she looked could trigger a crying fit.

A correct diagnosis for Rylae-Ann allowed us to better support her symptoms. (Photo by Richard E. Poulin III)
Ptosis, or looking sleepy with droopy eyes
When close friends could gain Rylae’s trust and see her happy state, they would ask if she had just woken up or commented that she looked sleepy. Taking passport and identification photos was challenging because the attendant instructed us to open her eyes. As you might imagine, the whole event was filled with us doing dances while Rylae wailed at the top of her lungs.
The droopy eyes and sleepiness went hand in hand. She was either crying or napping, though she was noticeably different and demonstrated her best movements after sleeping. We were able to capture moments of happiness, but we wanted answers, so we searched the internet for reasons why our sleepy baby was crying and having spells that strained her eyes and limbs.

Despite looking sleepy and having droopy eyelids, Rylae-Ann was awake and responsive. (Photo by Richard E. Poulin III)
Excessive sweating
We needed to place and replace blankets under our daughter throughout the day and night since she exhibited symptoms of excessive sweating and temperature instability. Even if it was cool outside or we had the air conditioning at the coolest setting, our daughter would continue to profusely sweat. We managed her sweating as best we could.

Regardless of the temperature, Rylae-Ann would excessively sweat, so we tried to keep her cool and dry. (Photo by Richard E. Poulin III)
The results of your search
Just because you landed on this page does not mean your child has AADC deficiency or any other disease with similar symptoms. However, it’s essential to recognize concerns and describe them accurately using medical terms. Information and specific terminology relating to your observations will support your medical team in correctly diagnosing or recommending testing.
If this column supported you in correctly diagnosing your child, don’t worry. There is a fantastic community of parents and caregivers ready to help.
Note: AADC News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of AADC News or its parent company, BioNews, and are intended to spark discussion about issues pertaining to aromatic l-amino acid decarboxylase deficiency.





Comments